HOW CLOZAPINE WORKS
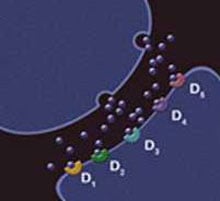
Scientists have made major breakthroughs in their understanding of the chemistry of the brain and how medications can help rebalance that chemistry. Prior to those breakthroughs, we had little knowledge of the role of the chemical messengers in the brain (called neurotransmitters) that affect our moods and our thought processes. Now, based on discoveries about the brain’s use of the neurotransmitter chemical dopamine, scientists have learned how to enable many previously unresponsive patients to lead more normal lives. (See neurotransmitter illustrations below.)
Clozapine is also used for reducing the risk of suicide in patients with schizophrenia or schizoaffective disorder who have attempted suicide in the past and may be at risk of suicidal behavior again.
Clozapine may work when other medications don’t
Doctors prescribe Clozapine for the management of patients with schizophrenia when they have not been helped by other medications (a condition called treatment-resistant schizophrenia).
Clozapine blocks a chemical called dopamine
 |
 |
 |
| Artist’s conception of the chemical messenger dopamine (shown as blue spheres) leaving one nerve cell and traveling to the adjacent nerve cell to occupy one of five possible dopamine receptors (D1, D2, D3, D4, or D5). | Clozapine (shown as orange spheres) is believed to relieve schizophrenia by temporarily occupying these same receptors and blocking the dopamine from having its usual effect. |
Clozapine is a prescription medicine used for treatment-resistant schizophrenia. Clozapine is also used for reducing the risk of suicide in patients with schizophrenia or schizoaffective disorder.
![]() IMPORTANT SAFETY INFORMATION
IMPORTANT SAFETY INFORMATION
-
Do not take clozapine if you are allergic or have had an allergic reaction to any of the ingredients of clozapine
-
Severe Neutropenia. Clozapine can cause severe neutropenia. Neutropenia is a blood disorder that occurs when a certain type of white blood cells called neutrophils are not made, or not enough of them are made. This makes it harder for your body to fight infections which could lead to serious infections and death. Before you can start clozapine and during treatment, you must have regular blood tests to measure the number of neutrophils you have in your blood. This test is called absolute neutrophil count (ANC). If the number of neutrophils, or ANC, is too low, you may have to stop clozapine. Your doctor will decide if or when you should restart clozapine. Immediately report any signs or symptoms of infection such as flu-like illness, fever, chills, tiredness or weakness, mouth sores; skin, throat, vaginal, kidney, urinary or lung infection (like pneumonia) to your doctor that occur any time while using clozapine
-
Clozapine REMS Program. Because of the risk of severe neutropenia, clozapine is available only through a restricted program called the Clozapine Risk Evaluation and Mitigation Strategy (REMS) program. This program is designed to ensure you have the required blood tests before filling your prescription. Prescribers, patients, and pharmacies must enroll in the program. Monitoring and reporting of blood work (ANC) is required. For more information, visit http://www.clozapinerems.com or call 1-844-267-8678
You will need to get your blood tested on the following schedule or as directed by your doctor:
- Weekly blood tests are required for the first 6 months you are taking clozapine
- An ANC is required every 2 weeks for the next 6 months if an acceptable ANC is maintained during the first 6 months of continuous therapy
- An ANC is required once every 4 weeks thereafter if an acceptable ANC is maintained during the previous 12 months of continuous therapy
-
Orthostatic Hypotension, Bradycardia, and Syncope. Clozapine can cause your blood pressure to drop suddenly, called orthostatic hypotension, which makes you feel dizzy or lightheaded and can lead to fainting (syncope) when you change position, such as standing or sitting up after lying down, especially when you first start taking the medication. Follow your doctor’s instructions exactly on how you should take your medicine. Contact your doctor immediately if you feel faint, lose consciousness, or have any signs or symptoms of low heart rate or abnormal heart beats
-
Falls. Clozapine may cause drowsiness, fainting when you change position, and other instabilities, which may lead to falls and, consequently, fractures or other injuries. Contact your doctor immediately if you feel overly drowsy, feel faint, lose consciousness, or have any of these symptoms.
-
Seizures. There is a risk of having seizures during clozapine treatment. Tell your doctor if you have a history of seizures or are at risk for seizures. While taking clozapine, you should avoid driving or any other activity where a sudden loss of consciousness could cause harm to yourself or others such as operating machinery, swimming or climbing
-
Myocarditis, Cardiomyopathy, and Mitral Valve Incompetence. Clozapine has caused cardiomyopathy (enlargement of the heart muscle) and myocarditis (inflammation of the heart muscle) which can cause death. The risk of having myocarditis is highest during the first month of treatment but can continue throughout treatment. Tell your doctor right away if you experience chest pain, an increase in heart rate, abnormal heart beats, shortness of breath, fever, flu-like symptoms, low blood pressure, swelling in your body, and/or congestion in your lungs, as these may be signs of those conditions. Mitral valve incompetence (heart valve not closing tightly) has also been reported in patients taking clozapine who have had cardiomyopathy. If you experience clozapine-related myocarditis or cardiomyopathy, you should not take clozapine again, unless your doctor determines the benefit is thought to outweigh the risks
-
Increased Mortality in Elderly Patients with Dementia-Related Psychosis. Elderly patients with a mental illness called dementia-related psychosis (have lost touch with reality due to confusion and memory loss) and who are taking antipsychotic drugs, such as clozapine, are at an increased risk of death. Clozapine is not approved for use in these patients
-
Gastrointestinal Hypomotility with Severe Complications. Clozapine can cause digestive complications ranging from constipation to severe intestinal blockage which can lead to hospitalization, surgery, and death. Tell your doctor about any potential symptoms of constipation including difficulty passing stools, incomplete passage of stool, decreased bowel movement frequency, nausea, abdominal (stomach area) enlargement or pain, or vomiting. Your doctor will test you for constipation before and during treatment with clozapine.
-
Eosinophilia. Clozapine use can cause eosinophilia, which is an increase in a type of white blood cell above the normal range. This usually occurs during the first month of treatment and has been associated with inflammation of the heart, pancreas, liver, colon and kidneys. If it is suspected, clozapine should be discontinued immediately
-
QT Interval Prolongation. Clozapine treatment is associated with abnormal heartbeats that can be life-threatening. Tell your doctor if you, or anyone in your family, have had any heart problems. You should not use clozapine with other medicines that are known to cause any heart problems. Notify your doctor if you feel faint, lose consciousness or have abnormal heartbeats
-
Metabolic Changes (hyperglycemia and diabetes mellitus, dyslipidemia, weight gain). Clozapine is associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include:
- Hyperglycemia and Diabetes Mellitus: Tell your doctor if you have diabetes or if you are at risk for diabetes (for example, obesity or family history of diabetes). Your glucose levels should be monitored at the beginning of treatment and periodically while taking clozapine as this medicine can cause an increase in your levels. Tell your doctor if you are very thirsty, urinate often, have increased hunger, or feel weak
- Dyslipidemia: Changes in lipid and cholesterol levels have occurred in patients treated with clozapine
- Weight Gain: Significant weight gain has also occurred with the use of clozapine and should be monitored by your doctor
-
Neuroleptic Malignant Syndrome (NMS). Clozapine can cause NMS, a condition that can be life-threatening. Tell your doctor right away if you have some or all of the following symptoms: very high fever, stiff muscles, shaking, confusion, sweating, or increased heart rate or blood pressure
-
Fever. While taking clozapine, patients have experienced a clozapine-related fever which is temporary and usually occurs in the first three weeks of therapy. Tell your doctor if you have a fever while on clozapine as it may be a sign of a more serious condition
-
Hepatotoxicity. Severe and sometimes fatal hepatotoxicity have been reported. Notify your doctor if you experience extreme tiredness, weakness, anorexia, nausea, or yellowing of the skin or eyes.
-
Pulmonary Embolism. Pulmonary embolism (blood clot in the lung) and deep vein thrombosis (blood clot in a deep vein, usually the lower leg) have occurred in patients treated with clozapine. Immediately contact your doctor if you have pain in your legs, shortness of breath, chest pain, or other respiratory signs and symptoms
-
Anticholinergic Toxicity. Clozapine should be used with caution if you have or had a history of constipation, urinary retention, are taking other anticholinergic medications, or have an enlarged prostate gland. Contact your doctor right away if you feel disoriented, experience blurred vision, dizziness, fever, dry skin or dry mucous membranes. Tell your doctor about all of the medications you are taking and if you have ever had any eye, prostate or colon problems
-
Effect on Judgement, Thinking or Physical Abilities. Clozapine can affect how you think or behave and/or your physical abilities, and may make you feel sleepy and less alert, especially during the first few days of treatment. Do not drive or operate heavy machinery until you know how clozapine affects you. Ask your doctor when it would be okay to do these activities
-
Tardive Dyskinesia (TD). Clozapine can cause TD, a serious, sometimes permanent, condition in which you have uncontrolled movements of the face or other parts of the body. The risk for developing TD can increase over time with more medicine, but can also develop within a short time and at low doses. There is no known treatment for TD, but it may go away partially or completely if the medicine is stopped. Tell your doctor if you have body movements you cannot control
-
Cerebrovascular Adverse Reactions. Clozapine may cause an increased risk of cerebrovascular side effects including stroke which may lead to death. Clozapine should be used with caution in patients with risk factors for cerebrovascular adverse reactions.
-
Reactions after Abrupt Discontinuation of Clozapine. If abrupt discontinuation of clozapine is necessary, your doctor should monitor you for psychotic symptoms and other side effects including profuse sweating, headache, nausea, vomiting, and diarrhea which can be signs of a more serious condition.
-
Common Side Effects. The most common side effects of clozapine are drowsiness, dizziness, lightheadedness, headache, trembling, fast heart rate, low blood pressure, fainting, excess saliva, sweating, dry mouth, vision changes, constipation, nausea, and fever
-
Missed Doses and Re-initiating Treatment. Do not stop taking clozapine without talking to your doctor first. If you miss taking clozapine for more than 2 days, you should not restart your medication at the same dosage but should contact your physician for dosing instructions
-
Use with Other Medications. Tell your doctor about all of the medicines you are taking, or plan to take, including any prescription, over-the-counter medicines, herbal products, or supplements. There is a potential that these drugs could interact with clozapine
-
Pregnancy and Nursing. Clozapine should be used in pregnancy only if the potential benefit is greater than the potential risk to the fetus. Tell your doctor if you are pregnant or plan to become pregnant. Do not breastfeed while taking clozapine
-
Phenylketonuric (PKU) Patients. Clozapine, USP Orally Disintegrating Tablets contain phenylalanine (a component of aspartame) and therefore if you have PKU, you should not take Clozapine, USP Orally Disintegrating Tablets
Call your health care provider for medical advice about side effects. You are encouraged to report side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
For Print Pieces: Please read the accompanying full Prescribing Information including Boxed Warning.
For Digital Pieces: Please read the full Prescribing Information, including Boxed Warning.




